Total Body Regeneration Starts Here
Now Offering IV PRP Therapy + Localized PRP Injections
Welcome to the future of healing
We're proud to introduce an advanced Regenerative Medicine Protocol, designed to activate your body's natural healing systems through Platelet-Rich Plasma (PRP)—delivered intravenously and through targeted injection.
5-Week Regenerative Protocol
Weeks 1–4: Preparation Phase – Stimulate & Support
-
Functional Assessment with Dr. Sulack or Dr. Rhea to develop a targeted treatment plan.
-
Organ-Specific Activation: Peptides tailored to your concerns—joints, brain, nervous system, immune system, digestion, kidneys, hormones, and/or muscles.
-
Weekly Cold Laser Therapy (635nm): Stimulates stem cell activity and supports healing through non-invasive light therapy.
Week 5: Regeneration Delivery
-
IV PRP Therapy: Delivers concentrated healing factors systemically to support whole-body recovery and inflammation reduction.
-
Localized PRP Injection: Precision-guided regenerative therapy into a specific joint (shoulder, knee, hip, etc.).
Recommendations:
- IV PRP therapy can be done indefinitely; a 4-cycle start is ideal.
-
Local PRP injections may be repeated in up to 3 cycles per joint.
What is Regenerative Medicine?
Regenerative medicine is a modern, research-backed approach that taps into your body’s healing potential. Unlike conventional treatments that suppress symptoms, regenerative therapies promote actual cellular repair and tissue regeneration.
We’ve helped patients address:
-
Chronic joint pain and arthritis
-
Ligament and tendon injuries
-
Bulging discs and soft tissue damage
-
Neurological dysfunction and brain injury
-
Persistent inflammation and fatigue
How It Works
PRP therapy uses your own blood’s platelets, concentrated and activated, to unleash powerful healing factors. Whether injected locally or administered via IV, PRP amplifies your natural healing response by:
-
Stimulating stem cell activity
-
Reducing inflammation
-
Promoting collagen and tissue repair
-
Supporting nerve and vascular regeneration
Instead of masking pain, PRP therapy instructs your body where and how to heal.
Backed by Science: Clinical Research on PRP IV Therapy
Though PRP injections are well-known, PRP IV Therapy is an emerging frontier—one with promising clinical data.
Systemic Recovery and Immune Modulation
-
Severe Illness Recovery: A 2021 study in Scientific Reports showed that IV-administered autologous activated PRP (aaPRP) improved outcomes in patients with severe inflammation by modulating immune response and speeding recovery.
➤ Read the study -
Neurological Benefits: A recent clinical review reported marked improvements in memory, neurocognition, and motor function in patients treated with IV PRP during post-COVID rehabilitation.
➤ See the case review
Joint and Soft Tissue Applications
-
Rotator Cuff & Shoulder Injuries: PRP outperformed traditional therapies in reducing pain and improving function.
-
Tennis Elbow: Meta-analyses showed longer-lasting relief with PRP compared to steroid injections.
➤ Read more -
Jumper’s Knee, Hip Labrum, and Plantar Fasciitis: All showed improved outcomes in tissue repair and pain levels with PRP use.
Full-Body Healing Potential
A review in Frontiers in Pharmacology found that PRP therapy enhances repair in muscles, ligaments, and tendons, especially when combined with laser therapy.
➤ Review the research
Ready to Revitalize Your Health?
Regenerative medicine represents a new era of healing—targeted, non-invasive, and rooted in the intelligence of your own biology. Whether you’re dealing with chronic inflammation, joint pain, or fatigue, PRP IV and injection therapy may be your path to lasting relief.
Schedule Your Consultation Today
Let’s build your personalized plan to heal, regenerate, and thrive.
Current Stem Cell Research
PRP (Platelet-Rich Plasma) Treatment:
"A non-surgical regenerative therapy (Bioactive Cellular Treatment) using your own blood (Platelet-derived Growth Factors)."
CLINICAL RESEARCH:
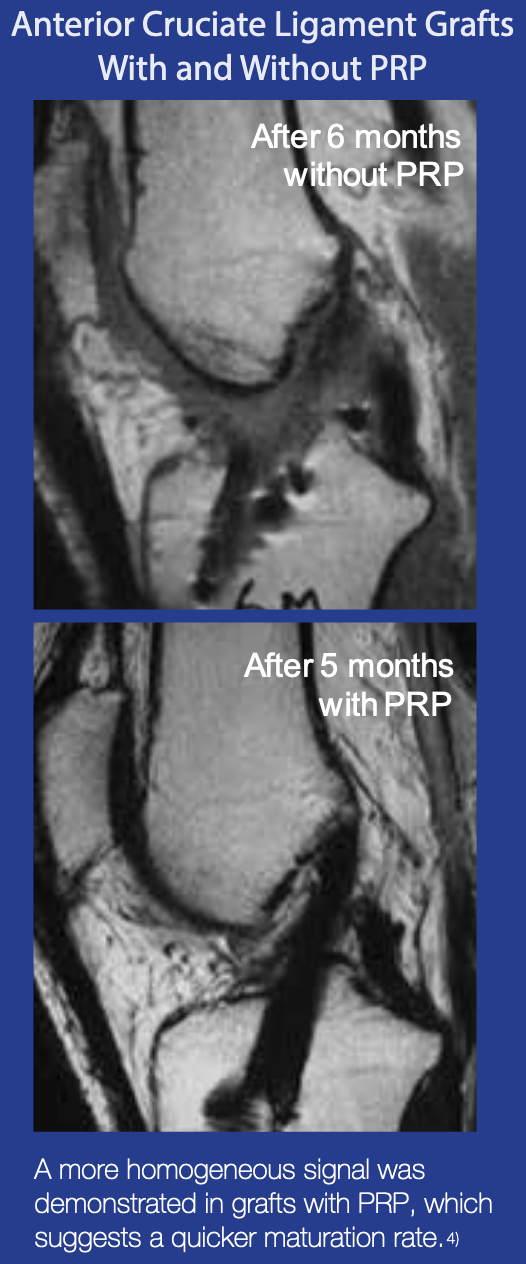
ACL (Anterior Cruciate Ligament) Grafts With and Without PRP
ACL reconstruction with the use of PRPG achieves complete homogeneous grafts assessed by MRI, in 179 days compared with 369 days for ACL reconstruction without PRPG. This represents a time shortening of 48% with respect to ACL reconstruction without PRP.
Radice F, et al, Comparison of Magnetic Resonance Imaging Findings in Anterior Cruciate Ligament Grafts with and without Autologous Platelet-derived Growth Factors,The Journal of Arthroscopic and Related Surgery 26, issue 1, 2010;50-57
Mishra, et al, Treatment of Tendon and Muscle Using Platelet-Rich Plasma, Clin Sports Med 28, 2009;113-125
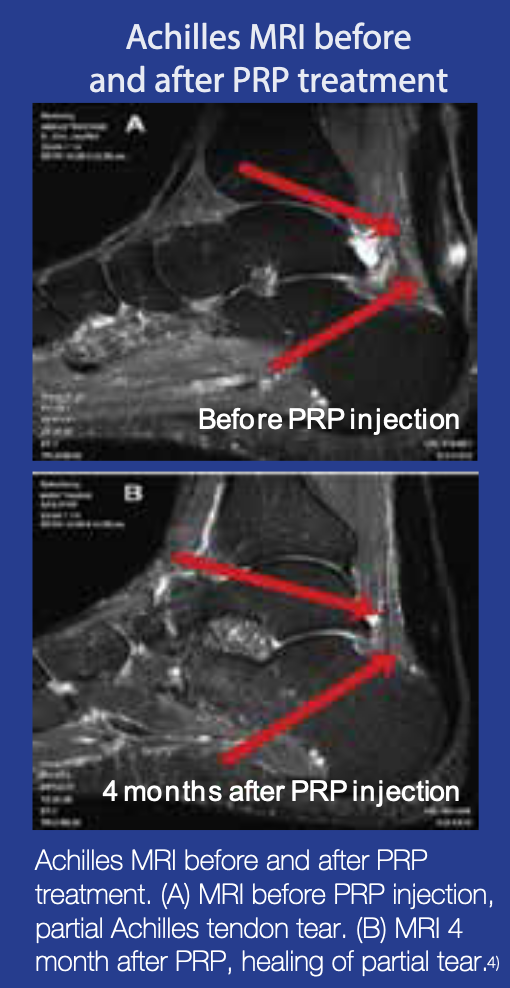
CLINICAL RESEARCH:
PRP Improves Chronic Tendinosis (Achilles)
PRP may improve tendon injuries as well as other chronic tendinosis. Specifically, it could be possible to treat an acute Achilles tendon tear non-operatively using a PRP injection.Non-surgical, ultrasound guided injection of PRP into the Achilles tendon within one month of injury, significantly improved a 90% Achilles tendon rupture in 6 weeks, leaving only a small focal tear. At 24 weeks, the tear was completely resolved.
Steven Sampson, et al, Platelet-rich Plasma Therapy as a first-line Treatment for severe Achilles Tendon Tear: a case report, International Journal of Therapy and Rehabilitation 18, 2011;101-106 (Link)
Wellington K, et al, Platelet-rich Plasma in Orthopaedic Applications: Evidence-based Recommendations for Treatment,J am Acad Orthop Surg 21, 2013;739-748
Other Clinical Studies:
Treatment With Platelet-Rich Plasma Is More Effective Than Placebo for Knee Osteoarthritis
A Prospective, Double-Blind, Randomized Trial (Link)
Sandeep Patel,MS, Mandeep S. Dhillon, MS, FAMS, Sameer Aggarwal, Neelam Marwaha, MD, FAMS, and Ashish Jain, MD Investigation performed at the Department of Orthopaedics and Department of Transfusion Medicine, Post Graduate Institute of Medical Education and Research, Chandigarh, India - The American Journal of Sports Medicine, Vol. 41, No. 2
The Effects of Platelet-Rich Plasma on Cartilage: Basic Science and Clinical Application
Platelet-rich plasma (PRP) is emerging as a biological therapy for the treatment of cartilageinjuries and for intra-articular application to address knee pain. Basic science studiesindicate that PRP stimulates cell proliferation and the production of cartilage matrix bychondrocytes and bone marrow– derived mesenchymal stromal cells and increases theproduction of hyaluronic acid by synoviocytes. (Link)
Lisa A. Fortier, DVM, PhD, Catherine H. Hackett, DVM, PhD, and Brian J. Cole, MD, MBA - Oper Tech Sports Med 19:154-159
Platelet Rich Plasma in Rotator Cuff Repair
Despite clinical success rates over 85%, persistent anatomic defects afterrotator cuff repair are common and depend on the size of the tear repaired. The etiologyof delayed or failed tendon to bone healing is multifactorial and biologic augmentationof a rotator cuff repair would be clinically desirable. Autogenous platelets containmany growth factors and are critical in the physiology of bone, soft tissue, and woundhealing. Growth factors present in platelets include TGF-B, FGF, PDGF, EGF, andVEGF. Centrifugation techniques have been developed to create platelet rich plasma(PRP). These PRP preparations are designed to concentrate platelets and the growthfactors they provide. PRP has been used to augment healing in various animal modelsas well as clinical situations in humans. (Link)
Seth C. Gamradt, M.D., Scott A. Rodeo, M.D., and Russell F. Warren, M.D. - Techniques in Orthopaedics: 22(1):26–33
Choice of intra‑articular injection intreatment of Knee Osteoarthritis: platelet‑rich plasma, hyaluronic acid or ozone options
In the treatment of mild–moderate knee OA, PRP was more successful than HA and ozone injections, as the application alone was sufficient to provide at least 12 months of pain-free daily living activities. (Link)
Tahir Mutlu Duymus · Serhat Mutlu · Bahar Dernek · Baran Komur · Suavi Aydogmus · Fatma Nur Kesiktas - Knee Surg Sports Traumatol Arthrosc - European Society of Sports Traumatology, Knee Surgery, Arthroscopy (ESSKA) 2016
Platelet-rich plasma as a nonsurgical treatment option for osteonecrosis
Avascular necrosis (AVN) is a progressive condition characterized by bone tissue cell death as a result of ischemia, which is most often seen in weight-bearing joints. The traditional treatment of this disease process in the hip includes surgical decompression and joint replacement. This case report describes a novel nonsurgical approach for treating advanced-stage degenerative AVN of the hip with the use of autologous platelet-rich plasma. The patient demonstrated significant functional improvements after this intervention without the need for further treatment except for physical therapy. The report suggests the potential utility of platelet-rich plasma for the treatment of degenerative AVN. (Link)
The Performance and Musculoskeletal Regeneration Center, Washington, DC PM R. 2012 Dec;4(12):1015-9. 10.1016
Complete resolution of avascular necrosis of the human femoral head treated with adipose tissue-derived stem cells and platelet-rich plasma
We report a case of a 43-year-old man with early stage (stage 1) avascular necrosis (AVN) of the femoral head treated with adipose tissue-derived stem cells (ASCs) and platelet-rich plasma (PRP). ASC-containing stromal vascular fraction was mixed with PRP and hyaluronic acid. This mixture was then injected into the diseased hip under ultrasound guidance. The affected hip was reinjected weekly with additional PRP for 4 weeks. The patient was followed-up with sequential magnetic resonance imaging (MRI) scans at 3, 18, and 21 months after treatment, together with Visual Analogue Scale (VAS) Walking Index, Functional Rating Index, Harris Hip Score, and Range of Motion (ROM) assessments. The patient's severe hip pain was considerably improved at 3 months after treatment, with pain scores, ROM and MRI showing near complete resolution of AVN. Pain scores, ROM and MRI at 18 and 21 months after treatment indicated complete resolution of AVN. This case represents the first evidence of complete resolution of early stage AVN of the hip following treatment with ASCs/PRP. (Link)
J Int Med Res. 2014 Dec;42(6):1353-62
Return to Homepage
